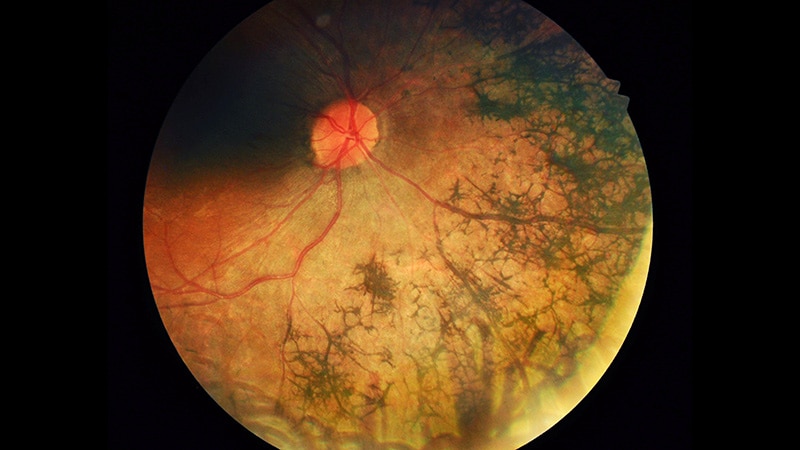
The prevalence of vision-threatening retinopathy in people with diabetes has increased exponentially in the past decade, most acutely among younger adults and Hispanic and Black populations, an analysis of a large electronic database has shown.
The cross-sectional analysis of 359,126 patients with type 1 and type 2 diabetes, published online on June 13, 2024, in JAMA Ophthalmology, found the prevalence of diabetic retinopathy (DR) increased 15% among the former and 7% among the latter between 2015 and 2022. In people aged 20-29 years with type 1 diabetes, the increases were more profound, rising almost fivefold, from 6.5 cases per 100,000 in 2015 to 30.7 per 100,000 in 2022, the researchers found. In those aged 30-39 years with type 1 disease, the prevalence almost doubled. In other age groups, the increase was more modest, ranging from 6% to 17%, and in those aged 70 years or older, the prevalence declined by 28%.
 Rishi Singh, MD
Rishi Singh, MDRishi Singh, MD, vice president/chief medical officer of Cleveland Clinic Florida Martin North and South Hospitals and a professor at Cleveland Clinic Lerner College of Medicine, Cleveland, said he and his colleagues expected to see an increase.
"We know that diabetes is increasing exponentially. We expected the rate of diabetic retinopathy to increase similarly," Singh told Medscape Medical News. But the magnitude of the jump in specific groups was "staggering," he added.
The study drew data from the US Collaborative Network within the TriNetX Analytics platform, a health research network that houses de-identified electronic health record data of more than 95 million patients in 56 US healthcare organizations.
Once vision loss occurs from DR, it cannot be recovered. Treatments with antivascular endothelial growth factor agents can preserve existing vision and prevent vision loss from worsening, but they cannot restore lost vision.
Most Impacted Populations
In people with type 1 diabetes, the cohort aged 20-29 years experienced sharp increases in prevalence across three dominant ethnic and racial groups: A 3.8-fold increase for Black populations, a 7.6-fold increase for Hispanic populations, and a 5.1-fold increase for White populations.
Men had greater increases than women, with White men having the greatest prevalence in 2022 — 38.6 cases per 100,000.
Among those with type 2 diabetes, the prevalence of DR rose 2.5-fold in the group aged 20-29 years and by 60% in the group aged 30-39 years.
Singh and his colleagues also observed "substantial race and ethnicity trends" within age groups, notably the younger cohorts. Hispanic men aged 20-29 years experienced a 5.1-fold increase in the prevalence of DR, whereas those aged 30-39 saw a 2.5-fold increase in the prevalence of the condition.
"By 30 years and older, the prevalence began to differentiate by racial and ethnicity groups, with Hispanic males and females having the largest prevalence followed by Black males and females," the researchers wrote.
Singh called the increase in the Hispanic and Black groups "incredibly concerning" and said it illustrates the effect of healthcare disparities. "Many of these patients in this category of ethnicity and race don't always necessarily always seek medical treatment," he said.
The findings point to the importance of screening for retinopathy at the time of a diagnosis of diabetes, Singh said, "It should start from outset, but we know from the vast majority of studies that have been done to date alas show that there's a lack of screening that's occurring in the population."
Even among people with insurance, screening rates are only 50%-70%, he said. "Even with the best insurance, the screening rates are not the highest," he said. "We hope we can get better screening, which would improve the ability to preserve vision in these patient populations, but thus far, it's not happening." During the study period, at least three glucagon-like peptide 1 receptor agonists had been approved for the treatment of people with diabetes, but their effect on DR trends are difficult to measure, Singh said. "They were really for those patients who had difficulties maintaining their diabetic status overall," he said of the drugs.
A Call for More Concern About DR
 David Rein, PhD
David Rein, PhD"Doctors, caregivers of people with diabetes should always be concerned about diabetic retinopathy, and these results suggest that maybe they should be even more concerned about diabetic retinopathy," David Rein, PhD, a senior fellow and program area director in public health at NORC, and coauthor of an invited commentary on the study, told Medscape Medical News.
The commentary noted that the Patient Protection and Affordable Care Act, which took effect in 2014, and the COVID-19 pandemic, during which a public health emergency provided health insurance to people who would otherwise have lacked coverage, may have factored into the increase in diagnosed rates of DR in the study.
"The emergency declarations, certainly among the Medicaid population and perhaps among other populations, may have made it so people kept their insurance when they wouldn't have had their insurance otherwise," Rein said. "Also, the Affordable Care Act went into effect and increased the number of people with insurance in the country, allowing more people to visit the doctor and be evaluated for diabetic retinopathy, when in the past maybe they would not have been."
The COVID-19 pandemic may have contributed in another way, he said, "The rates of all preventive healthcare declined in the pandemic, particularly during 2020, and so delaying of regular eye exams, delaying of potential treatment for diabetic retinopathy, and delaying medical visits for care of diabetes could've led to worsening of diabetes over time, which may have led to an increase in diabetic retinopathy."
Rein added that the study also demonstrated the power of using data from large administrative databases and electronic health record data sources. "What we really need are better population-based surveys of people in care and not in care to address the issue of potentially increasing rates of diabetic retinopathy," he said.
The study received funding from the Clinical and Translational Science Collaborative of Cleveland, Research to Prevent Blindness, and the National Eye Institute. Singh disclosed financial relationships with Genentech/Roche, Alcon, Novartis, Regeneron Pharmaceuticals, AsclepiX, Gyroscope, Bausch + Lomb, and Apellis Pharmaceuticals. Rein disclosed funding from the Centers for Disease Control and Prevention.
Richard M. Kirkner is a medical journalist based in the Philadelphia area.

.webp) 2 days ago
3
2 days ago
3
























 English (US)
English (US)