Please note that the text below is not a full transcript and has not been copyedited. For more insight and commentary on these stories, subscribe to the This Week in Cardiology podcast, download the Medscape app or subscribe on Apple Podcasts, Spotify, or your preferred podcast provider. This podcast is intended for healthcare professionals only.
In This Week’s Podcast
For the week ending May 3, 2024, John Mandrola, MD, comments on the following news and features stories: Transcatheter aortic valve implantation (TAVI) vs surgical aortic valve replacement (SAVR), more on renal denervation (RDN), inclisiran, and marketing disguised as science.
TAVI vs SAVR
Let’s start with the DEDICATE-DZHK6 trial, or just the DEDICATE trial from now on in this discussion.
German investigators at 38 sites (first author, Stefan Blankenberg), performed a randomized controlled trial (RCT) of TAVI vs SAVR in low- to intermediate-risk surgical patients with severe aortic stenosis (AS). DEDICATE is notable for many reasons: no industry funding and the operators could choose any TAVI valve.
It was a noninferiority (NI) trial with a primary outcome of death or stroke at 1 year. That’s a problem and I will come back to it.
In the introduction, the authors write that their trial had broad inclusion criteria, unlike the highly selective PARTNER 3 and Evolut Low Risk trials. They believe that DEDICATE will be more reflective of regular practice.
Exclusion criteria included patients with substantial coronary artery disease (CAD) and those with bicuspid aortic valves.
The trial enrolled about 1400 patients split evenly between the TAVI and SAVR arms. There was substantially more crossover (SAVR to TAVI) and withdrawal in the SAVR arm.
The mean age was 74 years. The median STS (Society of Thoracic Surgeons) score was 1.8%, which was similar to PARTNER 3 and Evolut-LR.
Two-thirds of TAVI were done with a balloon expandable valve (BEV) and one-third were done with a self-expanding valve (SEV). SAVR was done with full sternotomy in half the patients.
The primary outcome clearly favored TAVI.
5.4% primary events in TAVI vs 10% in SAVR. The absolute risk decrease was 4.6%; hazard ratio (HR) 0.53; 95% confidence interval (CI), 0.35 to 0.79; clearly significant for NI.
Death was 2.6% in the TAVI group vs 6.2% in the SAVR group (HR, 0.43; 95% CI, 0.24 to 0.73).
Stroke was 2.9% in TAVI and 4.7% in SAVR (HR 0.61; 95% CI, 0.35 to 1.06).
Pacemakers were performed in 11.8% and 6.7% of the patients, respectively (HR 1.81; 95% CI, 1.27 to 2.61).
Prosthetic-valve dysfunction was 1.6% in the TAVI group and 0.6% in the SAVR group (HR 2.44; 95% CI, 0.87 to 8.15).
Safety wise:
Bleeding was 4.3% in the TAVI group and 17.2% in the SAVR group (HR 0.24; 95% CI, 0.16 to 0.35).
Vascular access-site complications were 7.9% with TAVI vs 0.7%, with SAVR (HR 10.64; 95% CI, 4.84 to 28.94).
Comments. I commend the German investigators for doing a trial without industry support. Industry is not nefarious, but industry-supported trials may be more selective and certainly limit valve choice.
Trials are good. We should have more trials.
There are very curious findings in this trial, however. Despite a median STS score similar to the low-risk BEV and SEV trials, the primary outcome rate is many times higher in DEDICATE.
In DEDICATE, death or stroke was 5.4% (TAVI) vs 10% (SAVR)
In PARTNER-3, death and stroke were 1.8% vs 4.9% (S9 supplement).
In DEDICATE, death was 2.6% vs 6.2%.
In PARTNER 3, death was 1.0% vs 2.5%.
In Evolut LR, death was 2.4% vs 2.9%.
I do not understand why the rates of death/stroke events in DEDICATE were so much higher than in the PARTNER 3 trials, especially in the surgical arm.
I do not understand why surgical death was 6% at 1 year vs less than 3% in the PARTNER and Evolut LR trials. What’s going on?
DEDICATE authors posit that they enrolled patients during the pandemic. I don’t see that as a likely cause. They also note there were more women in the trial, but it was not that much more; 44% vs 36%. So that is not a likely explanation.
Another problem I have with this trial is 1 year follow-up. In the accompanying editorial, “Another Early Win for TAVI in Low-Risk Patients,” Dr Shah was relatively cautious in his closing words, but the title and bulk of the article were celebratory. Publication of the trial in the NEJM is itself celebratory.
You can love TAVI, as I do. It is an amazing advance. But there are now well-known patterns of events. TAVI performs better than surgery in the first year. But there is catch-up in the coming years.
A 5-year outcomes meta-analysis, first author, Fabio Barili, in the European Journal of Cardiothoracic Surgery, finds that when you look at 5-year results there appears to be no difference, but when you consider TAVI’s early advantage, TAVI performance from 2 to 5 years is worse than surgery.
Proponents of TAVI will point to the recent NOTION 8-year results, which found no difference in major outcomes. But I would remind you all that this included only 140 patients in each treatment arm.
The problem with over-enthusiastic use of TAVI in younger patients with AS is that we don’t have good long-term data. A 72-year-old person is going to make it to 80. When they have structural valve deterioration, then what? Given the terrible outcomes of removing TAVI valves, you commit this person to another valve-in-valve.
TAVI is a great innovation for older patients with higher surgical risk. It’s use in younger patients remains more complicated.
Trials with one-year follow-up are not helpful in sorting out this question. Publishing DEDICATE in the NEJM with a praising editorial has the effect of creating even more therapeutic momentum towards TAVI. I don’t like it—even though I like TAVI.
Renal Denervation
Speaking of too-short follow-up….
The TARGET 1 RCT of RDN using alcohol-mediated ablation technique was presented at the American College of Cardiology (ACC) annual meeting and made it into Circulation.
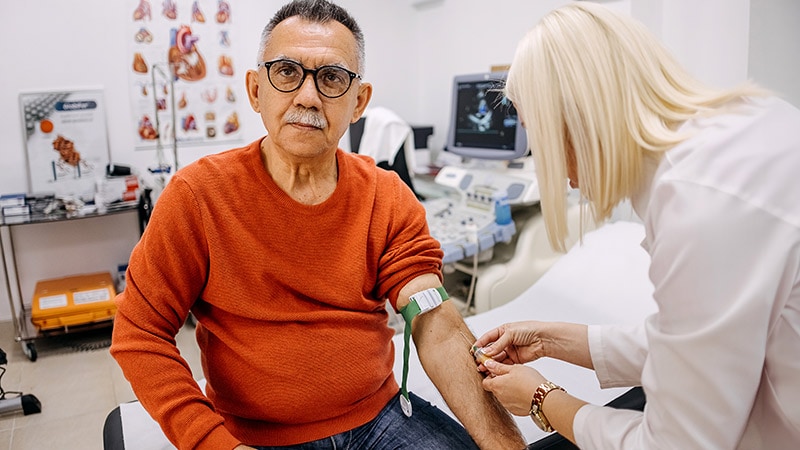
The idea behind RDN is interesting. You ablate sympathetic nerves and reduce blood pressure (BP). This could be huge because hypertension (HTN) is a huge problem, and many humans struggle to take pills on a regular basis.
Ultrasound and radiofrequency (RF) ablation devices have been approved, though I have opined previously that both are marred by modest reductions in BP, and lack of sham-controlled data beyond 6 months to a year. Of course, BP therapy is for decades.
Well, the investigators in the TARGET 1 trial had the idea of delivering alcohol into the perivascular space to achieve circumferential ablation of the afferent and efferent sympathetic nerves.
For the record, electrophysiologists can use alcohol within epicardial veins and, boy, does it ablate tissue. For ablation of atrial fibrillation (AF) we often inject alcohol into the vein of Marshall, and you see ablation in the region of the mitral isthmus up the anterior ridge between the left atrial appendage (LAA) and pulmonary vein. It is impressive.
However, in the sham-controlled TARGET 1 trial, wherein 300 patients were randomly assigned to sham or alcohol RDN, the mean ambulatory systolic BP reduction at 3 months, was only 3.2 mmHg. It was the same for office-measured BP.
The results made statistical significance, at a P-value of 0.0487, which makes me laugh that they carried it out to 4 decimal places.
One of the notable things about the results was that the sham-controlled arm got a 7 mmHg reduction of systolic BP. This, to me, emphasizes the importance of having sham-control arm.
The authors write about how patients were allowed to take up to 2 to 5 prescription medications. About 20% were on aldosterone blockers, and this may have mediated the modest results.
I don’t know, renal denervation is a great idea, but the reductions in BP are small. This trial provides extremely modest reductions at only 3 months. This is likely to get even lower with longer follow-up.
I’ve already seen adverts from hospitals and those unseemly social media pics where docs pose with shiny-happy-industry reps announcing their first procedure.
To me, these sorts of pictures are unprofessional, and I wish my colleagues would refrain from public celebration alongside industry.
In the matter of RDN, I am pessimistic but not close-minded. What would convince me is extending the sham-controlled follow-up. Proponents say it’s not possible. I disagree.
As for alcohol mediated RDN, this is the first half-mile of a marathon. There is much more work ahead.
VICTORIAN-INITIATE
Last week on this podcast, I spoke about surrogate markers. It was regarding a rather technical paper in JAMA on how surrogate markets often have dubious connections to overall clinical outcomes.
Today let’s go over an example of such a trial presented at the ACC meeting.
This was called the VICTORIAN-INITIATE trial, which made it into the Journal of the ACC as a simultaneous publication. I tell you about this trial for two reasons — one is to highlight the limitations of surrogate markers, and the other is to show you a marketing study that masquerades as science.
Inclisiran is a small-interfering RNA that inhibits hepatic PCSK9 production, which raises hepatic expression of the LDL receptor and increases LDL clearance. The ORION series of trials shows the twice-yearly injection lowers LDL cholesterol, but none of the ORION trials had clinical endpoints as a primary outcome. All we know is that the drug lowers LDL cholesterol.
Novartis, which makes inclisiran, benefits from the drug gaining US Food and Drug Administration (FDA) approval. But as far as I can tell, uptake is low, probably because of cost. Perhaps my colleagues are also worried that there are no clinical outcome data.
Anyway, a big inclisiran study was presented at ACC. You’d think the company would want to show that the drug reduces outcomes in patients with significant atherosclerotic cardiovascular disease (ASCVD).
Well, there was no such study. Instead, we got VICTORIAN-INITIATE, a trial of two strategies to get patients with established ASCVD who are not at goal LDL cholesterol to goal LDL cholesterol levels. Get this. Only 450 patients were randomized.
One group got inclisiran ‘first’ and the other group received standard of care, doctor’s choice, which may be nothing, ezetimibe, a PCSK9 inhibitor, or bempedoic acid.
And voila! Novartis succeeded in getting a positive trial. The “inclisiran first” strategy led to significantly greater reductions in LDL cholesterol from baseline to day 330 vs usual care (60.0% vs 7.0%; P < 0.001).
Statin discontinuation was not significantly different in the two groups. Novartis also won because they received positive comments from the floor at ACC.
The discussant of the study at the ACC meeting, Jorge Plutzky, MD, director of preventive cardiology at Brigham and Women's Hospital, Boston, Massachusetts, called this "an important study that provides another important example of stunning under-treatment of high-risk patients and coupled that with a really innovative approach."
I should also quote from JACC:
VICTORION-INITIATE was funded by Novartis Pharmaceuticals Corporation, First author, Dr Koren is an employee of a company that received PI fees for his participation in the Novartis VICTORION-INITIATE trial and that has received study grants and consulting fees from multiple manufacturers of PCSK9 inhibitors and other treatments for lipid disorders.Multiple authors had received funds from Novartis, and four of the authors are employees of Novartis.
Comments. I will concede a number of things. Inclisiran lowers LDL cholesterol via a PCSK9 mechanism, and a PCSK9 inhibitor has previously shown modest reductions in non-fatal CV outcomes. Inclisiran is easy to administer; twice yearly injections are nice. I also concede the causal role that LDL cholesterol has in ASCVD.
But LDL cholesterol remains a surrogate marker. Novartis has a lot of money. Why regulators did not compel them to do a trial powered for outcomes is hard to understand.
While it’s likely that inclisiran lowers CV events, we don’t know.
VICTORIAN-INITIATE could have enrolled 25 times more patients and then measured whether the extra LDL cholesterol lowering one gets with inclisiran results in a lowering of events.
As an aside, the trialists report event rates in this trial of about 2% in both groups. Obviously too few to say anything.
Without outcomes, we can say nothing about cost-efficacy.
I don’t get it. I don’t get why we allow unproven drugs on the market. I don’t get why ACC places such a marketing trial in high-profile status. And I don’t get why doctors are so accepting of low-evidentiary support. Why does bempedoic acid get studied in Clear outcomes, with its 13,000 patients and clinical endpoint, and inclisiran gets a pass? I am asking. Feel free to let me know.
Briefly
I am going to cut it short today because of my voice, but I want to point you to a provocative study in Circulation Outcomes , first author, Mathew Durstenfeld, in which they aimed to emulate a trial of early coronary angiography in patients with a new heart failure diagnosis. I am always interested in using observational data to try and emulate trials. Take a look.
Circulation also has an observational study drawing patients from the Women’s Health Initiative trial. This study finds an association between perfect systolic BP and better survival of older women. It has drawn the attention of some big names in cardiology, but I find aggressive BP therapy in the elderly a substantial area of harm.
Also, next week is the Heart Rhythm Society meeting. I will have a Hyde Park debate on LAA occlusion. Gosh, not again. If you are in Boston, come say hi.

.webp) 2 weeks ago
13
2 weeks ago
13






















 English (US)
English (US)