British investigators have demonstrated a "potentially curative" neoadjuvant regimen for early-stage germline BRCA 1/2–mutated breast cancer.
In a small trial, 39 patients randomized to the regimen — a combination of standard chemotherapy with the poly(ADP-ribose)polymerase (PARP) inhibitor olaparib — were alive at 3 years vs 39 of 45 (87%) randomized to chemotherapy alone.
"A remarkable 100% of patients were still alive at 36 months, which is a significant landmark for these patients," said chief investigator Jean Abraham, PhD, a breast oncologist at the University of Cambridge, Cambridge, England, who presented the findings at the American Association for Cancer Research (AACR) Annual Meeting 2024.
It's a "small but very powerful signal" of "what could be a potentially curative regimen that definitely does need to be confirmed in a larger study," Abraham added.
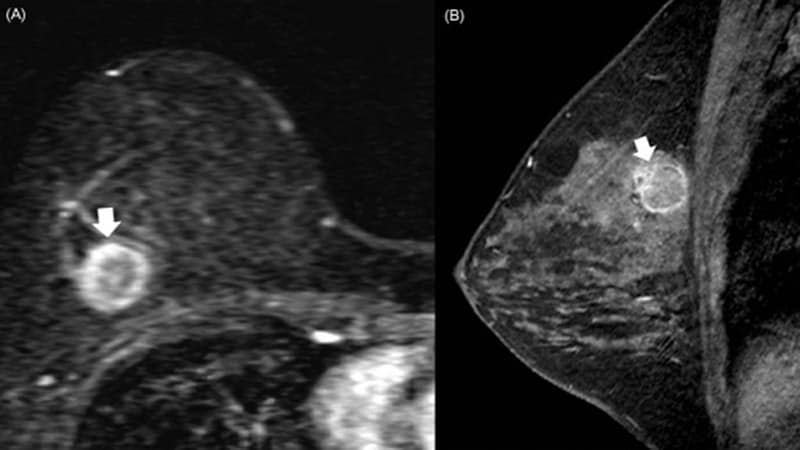
The study, a part of the PARTNER trial, included 84 patients with T1-2 tumors of any hormone status. Just over 70% in both arms had BRCA 1 mutations, and the rest had BRCA 2 mutations.
Past attempts at combining chemotherapy with PARP inhibitors have been hampered by excess bone marrow toxicity. To counter the problem, patients randomized to the combination therapy received olaparib 48 hours after carboplatin to give their bone marrow a chance to recover.
The median age was 38 years in the control group and 47 years in the olaparib arm. A greater proportion of patients in the control arm (42% vs 23%) had axillary node involvement.
Overall, patients received neoadjuvant carboplatin on day 1 and paclitaxel on days 1, 8, and 15 every 3 weeks for four cycles, followed by anthracycline every 3 weeks for three cycles. In the study arm, olaparib 150 mg was administered twice daily starting on day 3 continuing to day 14 during the first four cycles. Almost 90% of patients received at least 80% of their planned olaparib dose.
Despite the delay in olaparib dosing, 56.4% of patients in the combination arm required a transfusion vs 48.9% with chemotherapy alone.
At a median follow-up of 40.7 months, 96% of patients in the combination arm demonstrated event-free survival, with one patient relapsing, vs 80% in the chemotherapy-alone group, with nine patients relapsing.
In the final analysis, 64% of patients who received olaparib had a pathological complete response compared with almost 70% in the chemotherapy group, though the difference was not statistically significant.
The trial was stopped short at 50% enrollment after the data monitoring safety committee determined that olaparib add-on was unlikely to improve pathological complete response rates, the trial's primary endpoint.
However, pathological complete response rates did not appear to affect overall survival.
"It didn't seem to matter whether you had a non-pathological complete response, you still survived 100%" with the combination, Abraham said, adding that this is not the first study to show a disconnect between response rates and survival.
Perhaps, this disconnect could be due to "doomed cells" that look like residual disease but are, in fact, dying and unable to metastasize, she said.
No patients in the combination arm and two in the control arm received olaparib, immunotherapy, or capecitabine after surgery. Both control participants relapsed, and one died.
Toxicity was more severe for patients in the combination arm. More patients who received olaparib (76.9%) experienced a grade 3 or worse adverse event vs 60% of patients in the control arm.
Study discussant Hope S. Rugo, MD, a breast oncologist at the University of California San Francisco, highlighted a few limitations and remaining questions.
First, "this is a very small population, so small differences in the biology of the tumor, the patients, and even stage that we can't assess in the neoadjuvant setting could make a difference that would affect event-free and overall survival," she said.
Second, two patients with pathological complete responses relapsed in the control arm and died, "which is quite unusual," Rugo said. "Patients who achieve a pathological complete response generally have an excellent outcome."
Rugo also noted that "gap sequencing doesn't appear to avoid the toxicity of PARP inhibitors."
However, Rugo said, "the efficacy results are intriguing" and would need confirmation in a larger randomized trial, perhaps with newer, more selective PARP inhibitors.
The work was funded by AstraZeneca, maker of olaparib. Researchers included AstraZeneca employees. Abraham is an advisor to and disclosed grants, travel costs, and honoraria from the company. Rugo disclosed research funding from AstraZeneca and other companies.
M. Alexander Otto is a physician assistant with a master's degree in medical science and a journalism degree from Newhouse. He is an award-winning medical journalist who worked for several major news outlets before joining Medscape Medical News. Alex is also an MIT Knight Science Journalism fellow. Email: aotto@mdedge.com

.webp) 2 weeks ago
5
2 weeks ago
5





















 English (US)
English (US)