TOPLINE:
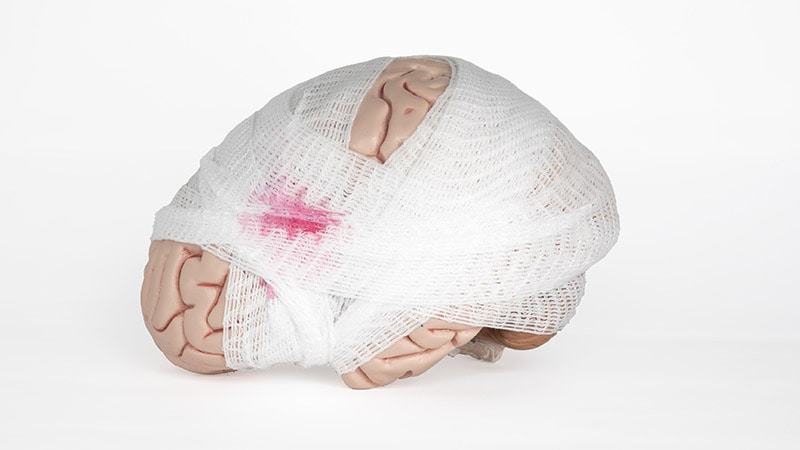
Seizure prophylaxis leads to a modest risk reduction for early posttraumatic seizure (PTS) in patients with mild or moderate traumatic brain injury (TBI).
METHODOLOGY:
- Researchers performed a meta-analysis of eight studies comprising 5637 patients with mild ( Glasgow Coma Scale [GCS] score, 13-15) or moderate (GCS score, 9-12) TBI in high-income countries, comparing rates of early PTS with and without seizure prophylaxis.
- Among these patients, 1541 received seizure prophylaxis, including levetiracetam, phenytoin and valproic acid.
- The primary outcome was the absolute risk reduction for early PTS, defined as seizures within 7 days of initial injury, in patients with mild or moderate TBI receiving seizure prophylaxis within the first week post injury.
- The secondary outcome was the absolute risk reduction for mild TBI alone, analyzed using five studies with 3803 patients.
TAKEAWAY:
- Seizure prophylaxis led to a 0.6% absolute risk reduction (P =.02) for early PTS in patients with mild to moderate TBI (GCS score, 9-15).
- Similarly, the absolute risk reduction for mild TBI alone was 0.6% (P =.04).
- The prevalence of early PTS was low, ranging from 0% to 4%.
- A total of 167 patients required treatment to prevent an episode of seizure.
IN PRACTICE:
"For patients with risk factors for early PTS as described previously, treating clinicians should consider instituting seizure prophylaxis," the authors wrote. "Practitioners should weigh low prevalence of early PTS and low risk reduction against risks of antiseizure medicine, including inappropriate long-term continuation," they further added.
SOURCE:
This study was led by Matthew Pease, MD, Department of Neurosurgery, Indiana University School of Medicine, Indianapolis, Indiana, and was published online on April 8, 2024, in JAMA Neurology.
LIMITATIONS:
The inclusion of six retrospective studies on seizures and only one prospective study could have introduced bias. The transfer of patients with severe injuries to level-1 centers might have limited generalizability. The absence of randomized clinical trials could have posed challenges for adequately powered trials. Tailored decisions by practitioners, such as prescribing seizure prophylaxis only to patients with more severe injuries, could have introduced bias and undermined the effectiveness of the prophylaxis.
DISCLOSURES:
Three authors reported receiving consulting fees from medical technology companies like Zimmer Biomet, NeuroOne Medical, and Neuroelectrics. One author reported receiving grants from the National Institutes of Health or National Institute of Neurological Disorders and Stroke, outside the submitted work. No other disclosures were reported.

.webp) 1 week ago
5
1 week ago
5























 English (US)
English (US)