Transthyretin (TTR) is a tetrameric serum protein that binds and transports thyroxine (T4) and retinol (vitamin A). TTR gene mutation results in misfolded insoluble extracellular protein deposition in blood vessels, tissues, and major organs. It is an autosomal dominant life-threatening disease with high penetrance.[1] Morie Gertz, MD, a professor and consultant at Mayo Clinic, talked to Medscape about hereditary amyloidogenic transthyretin (ATTR) amyloidosis.
What is a common initial presentation in a patient with ATTR amyloidosis?
There are two main ATTR amyloidosis phenotypes: neuropathy and cardiomyopathy. The patient will present with symmetric sensory and motor loss in their feet, and there may be pain if small nerve fibers are involved. Typically, a male patient between 60 and 70 years of age will report that they can't feel their feet or that it feels like they are walking on carpeting or wearing very thick-soled sneakers. The sensory loss ascends over time. Most cases of ATTR amyloidosis are diagnosed after 1 year of investigation[2], because these initial symptoms might be considered related to diabetes or alcohol misuse; often I see patients with an initial diagnosis of chronic inflammatory demyelinating polyradiculoneuropathy.[3] There are important red flags that the clinician should look for, such as bilateral carpal tunnel syndrome with median nerve compromise and autonomic neuropathy — intermittent diarrhea and constipation, overflow incontinence, sweating abnormalities, and orthostatic hypotension.[4,5] It is worth asking about family history; I sometimes find first-degree family members with a history of lower-extremity weakness interpreted as arthritis.
What are the initial diagnostic investigations recommended for these patients?
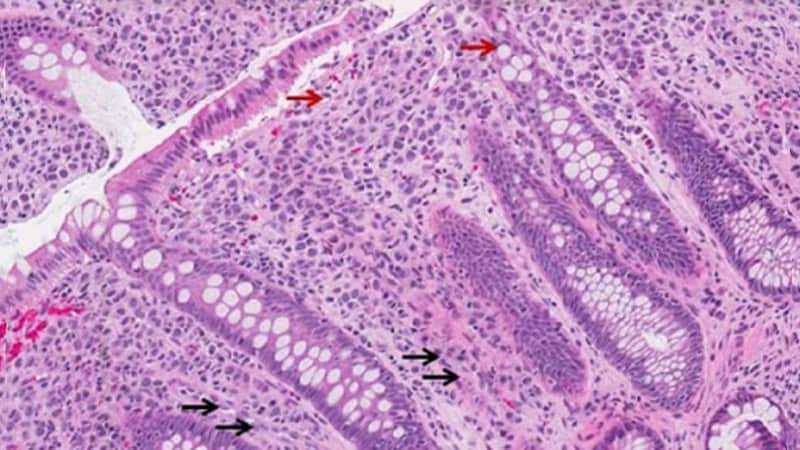
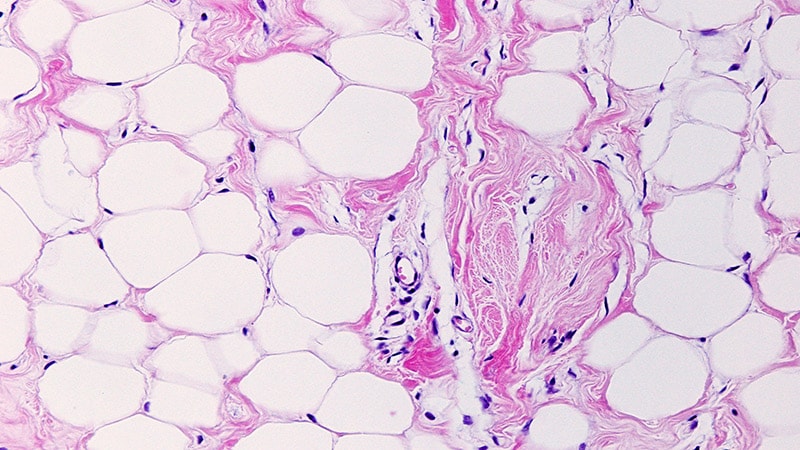
In most instances, patients will be referred to a neurologist with an electromyogram demonstrating a neuropathy. Here at Mayo Clinic, initial investigation for a patient with unexplained peripheral neuropathy with clinical suspicion of ATTR includes free light chain/serum and urine immunofixation electrophoresis, subcutaneous fat aspiration, and consideration of genetic testing for ATTR. It is crucial to rule out light-chain (AL) amyloidosis at this stage, which is not possible by clinical presentation alone. AL amyloidosis is a treatable condition, but patients can decline quickly.[6-8]
Is cardiomyopathy a later stage of ATTR amyloidosis?
There are all kinds of phenotypes: cardiomyopathy only, peripheral neuropathy only, and both at the same time. Usually, fibril deposition is synchronous in different tissues. Whether a patient will present to a cardiologist or to a neurologist will depend on which set of symptoms dominate. Signs and symptoms of a multisystem and multiorgan disorder are relevant clues. A neurologist may see a patient with neuropathy, fluid retention, and atrial fibrillation. Similarly, a cardiologist may see a patient presenting with heart failure with preserved ejection fraction and bilateral carpal tunnel syndrome or bilateral loss of sensation in their feet.[3,9] ECG findings include a disproportion between left ventricular wall thickness and QRS voltages, and the echocardiography will show thickening of the ventricle in a patient without a history of hypertension or hypertrophic cardiomyopathy. Nuclear imaging with bone scintigraphy (99mTc-3,3-diphosphono-1,2-propanodicarboxylic acid [DPD] or 99mTc-pyrophosphate [PYP]) may be diagnostic of ATTR amyloidosis, if it shows a strong uptake. It is worth mentioning that Doppler echocardiographic studies may show diastolic relaxation abnormalities, and cardiac MRI with gadolinium enhancement can show a very specific pattern in cardiac amyloidosis that experienced echocardiographers call the "cherry on top," which reflects severe impairment of global longitudinal strain.[10]
Should the clinician consider biopsy and genetic testing at this stage?
If monoclonal immunoglobulin or light chain are present in a patient with a positive cardiac scan, a biopsy is required to confirm or exclude the diagnosis of AL amyloidosis.[11] If an ATTR amyloidosis diagnosis is confirmed, genetic testing is strongly recommended. Different agents for ATTR treatment have been approved by the US Food and Drug Administration on the basis of whether it is wild-type ATTR or hereditary ATTR. It is estimated that 3%-4% of African American persons in the United States have a genetic mutation for ATTR amyloid, so it is possible that you are going to see this type of patient. If the ATTR is hereditary, a genetic counselor should be involved to counsel patient and their families on follow-up and surveillance of an autosomal dominant condition.[12]
There is more incentive to identify patients with ATTR amyloidosis owing to advancements in treatment. Can you tell us more about these developments?
For patients who have a cardiac phenotype, TTR stabilizers prevent protein misfolding and deposition, with a very low toxicity profile.[13] For patients with hereditary ATTR neuropathy with or without cardiac involvement, there are gene silencing treatments that prevent the TTR from being made in the liver, with great improvements in neurological impairment, quality of life, and survival.[14] Similar to other treatments with TTR synthesis inhibitors, we must supplement these patients with vitamin A. A phase 3 study on a CRISPR-based therapy to edit the mutated gene proposes to be a potentially new "one and done" treatment and is recruiting both wild-type and hereditary ATTR patients.[15] Interventions aimed at depleting existing amyloid deposits are also promising.[16] The goal is to remove existing amyloid by activating macrophages in these tissues. I think that's very exciting as we move forward.

.webp) 2 weeks ago
6
2 weeks ago
6





















 English (US)
English (US)