Hello. This is Dr JoAnn Manson, professor of medicine at Harvard Medical School and Brigham and Women's Hospital. I'd like to talk with you about our recent report in JAMA from the Women's Health Initiative (WHI) randomized trials and their clinical messages.
The WHI is the largest study of women's health ever done in the United States. Previous WHI clinical trial reports focused on the individual WHI trials of hormone therapy, calcium, vitamin D, and low-fat diet modification without a specific focus on translation to clinical practice. This new recent report summarizes the key findings of all randomized trials from the intervention phase, as well as long-term follow up, with a special focus on implications for clinical practice.
Hormone therapy. The findings show that women in early menopause (< age 60 years) had a lower absolute risk for adverse events from hormone therapy and generally had a more favorable benefit-to-risk profile than did women in later menopause. Overall, for women in their 60s and 70s, the investigators state clearly that the WHI findings support the use of hormone therapy for the treatment of moderate to severe or bothersome hot flashes, night sweats, and other menopausal symptoms in women in early menopause without contraindications. This is a US Food and Drug Administration (FDA)–approved indication for hormone therapy. The WHI findings really should never be used as a reason to deny the use of hormone therapy to women who are presenting with bothersome vasomotor or other menopausal symptoms and seeking treatment, especially when they are in early menopause and free of contraindications.
On the other hand, the WHI findings do not support the use of hormone therapy for the express purpose of trying to prevent heart disease, stroke, dementia, or other chronic diseases. That was the main purpose of the WHI trials: to evaluate menopausal hormone therapy for the benefit-to-risk profile when used for prevention of chronic diseases. The bar is set very high for using medications for prevention purposes, and the risk needs to be extremely low. But the findings are very consistent with the FDA-approved indications for treatment of menopausal symptoms among women in early menopause.
Calcium and vitamin D supplementation. Most previous trials of calcium and vitamin D supplementation had been done in women at increased risk for osteoporosis (those with low bone mineral density, a diagnosis of osteoporosis, or prior fracture). The WHI was the first randomized trial of calcium and vitamin D for fracture prevention among women at typical risk for fracture. The findings do not support the routine or universal use of calcium and vitamin D supplementation for prevention of fracture in all postmenopausal women.
However, the findings do support the use of supplementation for women who have nutritional gaps in intake and are not meeting the national guidelines for calcium and vitamin D intake. For example, the Institute of Medicine recommends calcium 1200 mg/d and vitamin D 600-800 IU/d as the recommended daily intake among postmenopausal women. So, supplementation is very reasonable to help meet these nutritional guidelines.
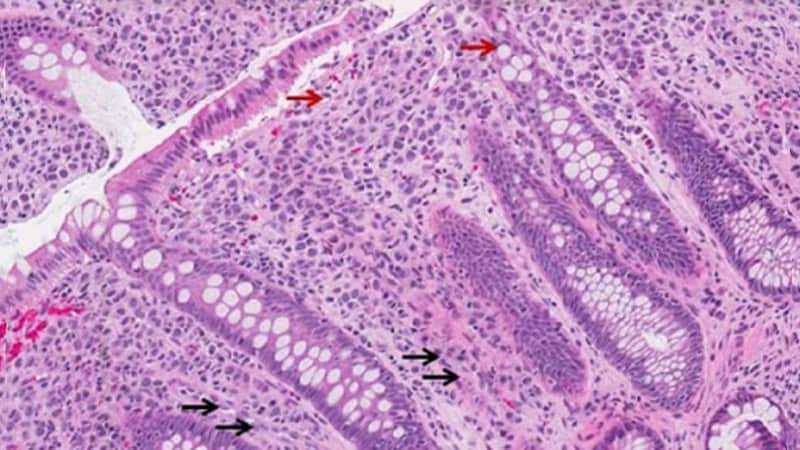
Low-fat diet. The low-fat modification trial included a reduced fat diet as well as an increase in fruits, vegetables, and grains. This dietary pattern did not significantly reduce the risk for the primary outcomes of breast or colorectal cancer. However, with long-term follow-up, there was a significant reduction in breast cancer death. So, this dietary pattern does provide an option for women who are at increased risk for breast cancer who are seeking to reduce these risks, and it would be very reasonable to recommend this diet in that scenario.
Overall, the findings do not suggest a one-size-fits-all answer for these interventions. They should not be universally recommended to all postmenopausal women. However, some women did benefit from these interventions, so the findings underscore the importance of individualized and personalized healthcare together with shared decision-making with the patient.

.webp) 1 week ago
5
1 week ago
5























 English (US)
English (US)