Xiuning Le, MD, PhD: Hello. I'm Xiuning Le. I'm an associate professor at MD Anderson Cancer Center in Houston, Texas. I'm a thoracic medical oncologist.
Joining me today are two experts, one from China and one from the United States. First is Dr Yi-Long Wu. He's very famous. He's the director of Guangdong Province People's Hospital, and he's also from Guangdong Lung Cancer Institute.
Our US expert is Dr Sandip Patel. He is a professor of medicine at University of California, San Diego.
Today we're speaking at the 2024 ASCO Annual Meeting in Chicago. It's a really busy meeting, and we have a large amount of new, exciting data reported out for targeted therapy, especially in the lung cancer space.
Let me begin to talk about some of the data that we have recently seen. I will try to group them into topics so that we can have a more informed discussion. First, let's dive into the antibody-drug conjugate (ADC) data that we saw very recently in three back-to-back presentations.
Sandip, can you please give us a quick summary of the results we saw?
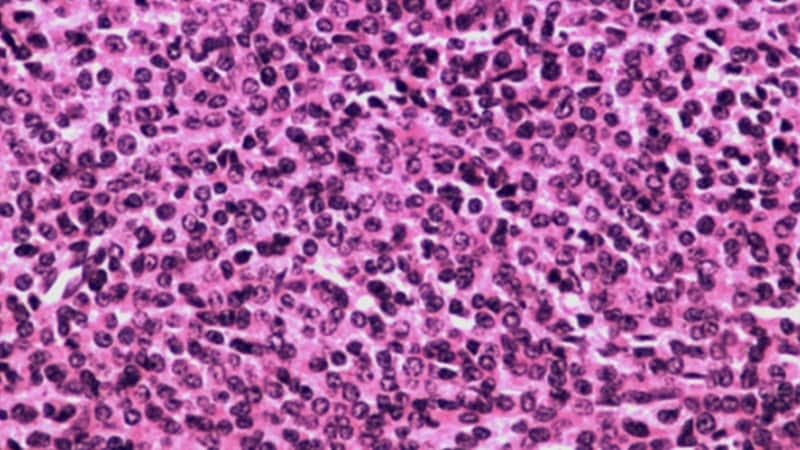
Sandip P. Patel, MD: I think we've really had a renaissance in ADCs. These are antibodies, through novel linker chemistry, with multiple cytotoxic payloads delivering chemotherapy directly to the tumor. We have multiple different combination studies that we saw today in thoracic oncology.
The first was the ICARUS-LUNG01 study. This was looking at datopotamab, which is a TROP2-targeting ADC. This is really around the biomarker story because one of the things is, while for antibodies, we have reasonable biomarkers for immunohistochemistry, for example, for ADCs, the biomarker story really hasn't been that clean. Even for HER2, HER2-negative patients can respond.
This is really an effort at describing and better understanding the biomarker story for datopotamab in lung cancer. I congratulate the investigators on some really interesting correlative work, which may define future biomarker selection for studies.
We also had an ADC and a PD-1 combination, the EVOKE-01 study, with sacituzumab govitecan. This is used in breast cancer in the United States, bladder cancer, and now it's being investigated in non–small cell lung cancer. We saw some provocative data in combination with a PD-1 antibody, especially in PD-L1–negative patients, so is this an opportunity to make cold tumors hot, so to speak.
The OptiTROP LUNG01 study, which is a next-generation TROP-2 ADC from Asia that's combined with a PD-1 inhibitor, in my opinion, showed really interesting data across PD-L1 strata. I'm looking forward to seeing how this data translates to the benefit of patients.
What are some of the antibody approaches you're most excited about in your clinic?
Le: Yi-Long, can you please make a comment on your experience with ADCs, and do you think ADCs will be just hype and then become not as exciting over time?
Yi-Long Wu, MD: No doubt, the ADCs are very topical in the oncology field, especially for lung cancer and breast cancer. So far, we also know the HER2 ADC drugs are very successful in breast cancer and lung cancer.
It's interesting if we think about why only the HER2 ADCs are successful and the others are unsuccessful. I think this is very important. I don't know why the other ADCs are not so successful. Maybe one of the reasons is due to the target population based on the antibody and the targets. I think we have the target, but we have an unselected population.
Le: There is a mismatch.
Wu: It may be the reason why so many ADC drugs so far have been under our expectations.
Le: Sandip, what do you think about the promising data of the TROP-2 ADC from Asia in combination with the PD-1 in the frontline setting? I think the data numerically looked very exciting. Do you think a combination with IO will be the direction to go?
Patel: I think so. I think the concerns around the emergent toxicities from ADCs, including lung toxicities such as interstitial lung disease, and how to deconvolute these from immune pneumonitis, are going to be very important. We know from small-molecule EGFR inhibitors that combining those with PD-1 has led to high rates of pneumonitis. How we avoid that as we deal with monoclonal-based strategies, I think, is going to be key.
The other thought — I think this is a great point — is that the biomarkers for ADCs don't seem to predict response as well as biomarkers for the bland antibody. There's some sort of synergy from this bystander payload effect that we don't yet have a biomarker to measure.
Le: Absolutely. They need more research going forward.
Wu: I think one of the issues is when the small molecule meets the ADC for patients with the driver gene mutation.
Le: I think people are excited about the ongoing clinical trials, basically double blockade, double targeting. I'm looking forward to seeing both efficacy and toxicity data. There is on-target toxicity, for example, for HER2 cardiac issues, and we'll have to see the data.
Wu: I always think that's very important. We always need to see the efficacy and the toxicity.
Le: Let's move on to a more specific patient population. At ASCO, we're hearing about EGFR mutation–related progress in the field. As you know, EGFR mutations happen in Asian populations more significantly. Now, we not only have small-molecule inhibitors but we are starting to see bispecific antibodies and maybe some immune modulation going into that space.
Sandip, can you give us a brief update of what we have seen at ASCO?
Patel: I think it's been a very exciting time in EGFR biology. One point is we can't treat these patients successfully if we don't test and do appropriate molecular testing. To me, there are at least three groupings of EGFR mutations. There are canonical mutations, exon 19 L858R — of course, your institution has done a large amount of work on this — secondarily, exon 20 insertion mutations, and then third are the atypical mutations, often in exon 18, and sometimes these are compound.
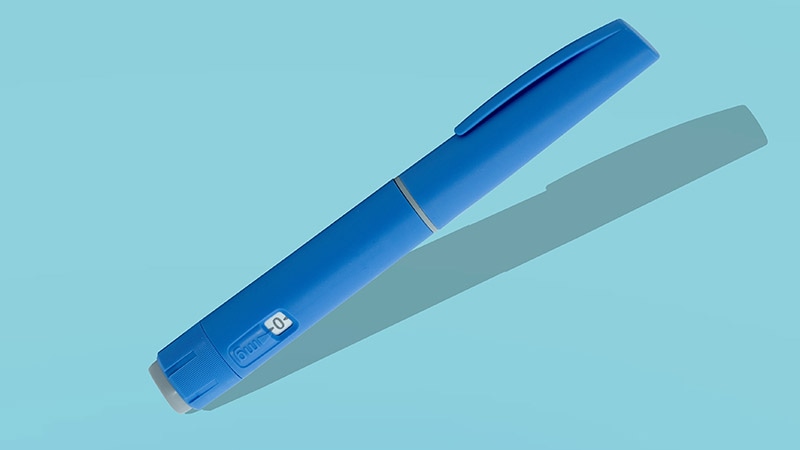
It's important to give not only the street name but the full address. It's not enough to say someone's EGFR positive anymore because that doesn't give us enough information because there are so many therapeutic strategies, as you nicely summarized. I think for the bispecifics, in particular, amivantamab, which is an EGFR-MET bispecific, we saw multiple interesting datasets.
Probably the most instantly practical are the results of PALOMA-3 using a subcutaneous version of amivantamab, which has an easier infusion schedule of less than 5 minutes rather than 5 hours, with less infusion reactions. I think it's a day-one change that's going to happen.
I think we saw some really provocative data around atypical mutations and combinations of amivantamab and lazertinib, which is a small-molecule EGFR inhibitor. Because many times, patients with atypical mutations, if they're treated with the current FDA-approved therapy, afatinib, especially for the PAC mutations, brain metastasis can be an issue. Lazertinib is a CNS-penetrant EGFR inhibitor.
We also saw the MARIPOSA frontline data, for canonical EGFR exon 19LA5 mutations, with amivantamab/lazertinib vs osimertinib showing a PFS benefit across all subgroups. I think it's going to be interesting to see how the overall survival data emerge, especially because so many patients in the US go from osimertinib to chemotherapy plus amivantamab in that setting.
Le: Yes. There have been many advances. Yi-Long, is amivantamab available in China yet? That's a naive question.
Wu: Amivantamab is not yet available in China. When we are looking at all the data we have seen in the EGFR-mutant patients, now maybe we have better tools and the direction would be better. The first is combination treatment. The second targets the patients who fail EGFR TKI treatment.
Le: Yes.
Wu: This is the HARMONi trial and also IO in these patients. When we look at the research, we find that if we are in the front line, the combination may have acceptable toxicity to get the PFS result. I think in this situation, in my mind and also in most of the patients', they like the combination with the better toxicity of the drug. This is one point.
The second point is that, after EGFR failure, the mechanism is very, very complex. We are increasing the so-called on-target mutations, all the EGFR amplifications. Another is the c-MET amplification.
It's very, very complex. In this complex situation, when we are using one model to treat every patient, I have some doubt that this is successful or not.
Le: Yes, absolutely. Sandip, can you also comment and follow up on Yi-Long's discussion of toxicity and the efficacy benefit? Also, high-risk biomarkers — we've heard a little bit about that. Can you please comment on how you feel about that data?
Patel: There are multiple high-risk biomarkers. Some of these are static — for example, baseline presence of p53. Others are more dynamic — for example, after a month of treatment, you still shed circulating tumor DNA at a high level.
When we think about these high-risk groups for canonical EGFR mutations, thinking about intensification strategies may be important. Now, whether it's these baseline factors or it's these dynamic factors after a month, I think we have some studies with data that remain to be seen.
Xiuning, we talked about EGFR-MET bispecifics. I think that's a very hot area based on the biology. But we've also seen some bispecifics that are immune mediated — for example, VEGF/PD-1 targeting. I'd love to hear your thoughts. We've had a history of VEGF targeting in EGFR mutations. What are your thoughts on the HARMONi-A study in these kinds of approaches?
Le: This year, Dr Zhang Li, also from Guangzhou, reported HARMONi China data. Those are the population post-EGFR TKI and the patients need chemo. The comparator arm is chemo, but the experimental is chemo plus a bispecific PD-L1 and VEGF. The study was positive and the hazard ratio was less than 0.5. It shows high promise.
Even the OS demonstrated a trend toward improvement of benefit. I personally think it is a very valid strategy for patients after TKI failure. In terms of toxicity, it is very well tolerated. After TKI resistance, we probably should filter out the driver-related mutations. For example, a fusion, or as Yi-Long was talking about, EGFR secondary mutation and MET amplification. For the rest of the patients, the majority, we don't know their resistance mechanism. I think a blanket approach to capture all is reasonable.
In the US, we also have to interpret that data with MARIPOSA-2, which is chemo plus amivantamab, currently going through a regulatory process. Patients have more options, which is good.
Let's move on to a different patient population. This is ALK and ROS rearranged lung cancer. In the ALK space, we have been seeing a good collection of TKIs to help the patients. Very impressively, this year, we saw updated data in the 5-year report.
Sandip, please give us a summary of the results, and then Yi-Long, please comment. How excited are you?
Patel: I thought it was a really great presentation. Sometimes, you see only new data. These data were so good at the 5-year mark that it basically got re-presented as an oral. This was the CROWN phase 3 international study of lorlatinib vs crizotinib in the frontline setting for patients with metastatic ALK-rearranged non–small cell lung cancer.
This is a drug that has been approved in the United States for use. It's had really phenomenal data, in my opinion, in the CNS in particular, both in terms of treatment and prevention with some of the best hazard ratios we've seen of any targeted therapy approach. There are certain neurocognitive side-effect issues that folks have to be aware of, and dose adjustments can mitigate those, but I've not found them to be a major headwind in my practice once you realize you can make dose adjustments and you educate the patients to be aware of them.
I really thought what's old is new again, and I think we saw excitement around this data because our ability to generate small-molecule inhibitors against fusions is one of the better targets that we've seen and the better drugs that we've seen in that setting. The ability to prevent brain metastasis, which is really a devastating side effect for these patients, I think, was key.
We also saw some additional data with lorlatinib in the ROS1 setting.ALK and ROS1 are very similar in terms of where they are in the kinome in targeting, and so the drugs they target are very similar as well. The ability to have a CNS-penetrant TKI that has this durability of response is really provocative and I think something folks need to consider. As we're thinking about managing toxicities, awareness and dose reductions can be key.
We have a wealth of riches in the ALK space with multiple potent inhibitors, including alectinib, brigatinib, and lorlatinib. What is your approach to these things?
Le: Also in China, we have ensartinib.
Wu: I think this kind of study is very, very exciting. First, it's only one drug. And after 5 years, the median PFS is not reached.
Le: Absolutely. Even the PFS is now hitting the 5-year mark. Really this is a beautiful example of how precision oncology can really impact our lung cancer patients' lives. The ALK patients are generally diagnosed very young. This is really just a game changer for the entire space.
Wu: The second point, I think, is very interesting. It's very important about the brain metastases. The lorlatinib either treated the brain metastases or prevented it. The data show that without the brain metastases at baseline, at 5 years…
Le: It's almost flat.
Wu: Yes. So I think it can prevent.
Le: Yi-Long, let me ask you this. Do you think EGFR and others — for example, K-RAS and BRAF — ultimately will have better TKIs to be just like ALK?
Wu: I think maybe this will relate to the biology for the subtype of lung cancer. In January, we called ALK fusion the so-called "diamond mutation" because we can treat this cancer. Finally, I think, this study also showed that even after 5 years of patients taking the drug, the side effects are under control.
Le: Yes.
Wu: We were very worried about the brain.
Le: Cognitive [side effects].
Wu: Now, we are like, oh, this is still okay, and we are not so worried about it. I think this is an amazing result.
Based on the result, we'll also consider, for some of the patients, having a drug holiday. We need to consider this — maybe at 10 years?
Le: I don't know. It's a mixed feeling, right? I think patients are so psychologically dependent on the drug. I don't have a single patient ever miss a pill for either ALK or EGFR. That's their safety blanket.
Patel: Xiuning, I'd love to hear your thoughts on clinical selection. In the CROWN data, they showed V3. There are three variants for ALK, of which V3 is a more aggressive and more resistant phenotype historically. There's also some data on P53, which is one of the historic higher-risk mutations.
Do you have a genomic assay? Do you think it's important to consider those molecular aberrations as we think about which ALK small-molecule inhibitor to utilize?
Le: Currently, I'm not, because I'm using lorlatinib frontline for my patients. I felt like also over time, the TKIs are so potent. For example, in the EGFR space, newer TKIs can hit exon 20, both the near loop and the far loop. Some of those distinctions might be not as important clinically compared to preclinical understanding nowadays.
However, P53 is still a bad player. We are seeing some of the phase 1 data trying to mitigate the TP53 MDM2 pathway. Maybe one day, we'll do some combination or interval treatment. That will be very interesting as well.
Wu: Even the PFS is not reached, but we are also finding that at 2 years, over 30% of the patients also relapsed. I think maybe the next direction we need to take is through bioinformatics to analyze which patients are not so good for responses, and then, for these patients, we need to give the strongest treatment.
Another thing that we are thinking about is the patient who goes even longer without relapse. Maybe for this patient, after 3 or 4 years, we should give them a drug holiday.
Le: Sandip, what's your final comment? I think Yi-Long talked about drug holidays and high-risk patients. What's your final comment?
Patel: I think we're all going to need a holiday after seeing all the great data at ASCO. It really is drinking from a fire hose, but it's important for our patients and it's important for patients to see how much progress we've made. The mortality for cancer has decreased in the United States and worldwide over the past several years, and it's due to precision oncology, particularly in lung cancer, which is the biggest killer among diseases.
When we're talking about these abstracts, it's important to understand that patients go on these studies and they volunteer at a point in their lives that they're really vulnerable. To see that translated into benefit for other patients, and hopefully themselves, is key. I think much of this is driven by precision oncology methods.
The ability to do molecular testing — there's liquid biopsy or tissue biopsy — is just so key. We wouldn't treat breast cancer without knowing ER/PR/HER2. We can't treat non–small cell lung cancer without knowing the molecular profile. This is, I think, a global issue as much as it is an issue in the US. I think artificial intelligence and digital pathology will hopefully liberalize some of these as well.
It's an exciting meeting. It's been exciting discussing all these late-breaking abstracts and things that I want to take back to clinic and try to utilize. Xiuning, what are your final thoughts?
Le: I do feel like in lung cancer, both incidence and mortality are decreasing globally, which is fantastic. I have started to encounter some younger patients in the clinic and I think that's a trend for some other solid tumors as well. I want even young patients to be aware, and I think we're moving to earlier and earlier discovery and screening. I hope we can one day cure cancer or have lung cancer as a chronic disease.
Thank you for joining us today. This is Xiuning Le, Sandip Patel, and Yi-Long Wu. We are speaking from the 2024 ASCO Annual Meeting in Chicago. Thank you for your attention.

.webp) 2 days ago
3
2 days ago
3





















 English (US)
English (US)