Tardive dyskinesia (TD) is a hyperkinetic movement disorder usually associated with the prolonged use of dopamine receptor–blocking medications. TD can vary from mild to severe, even disabling or life-threatening, significantly affecting a patient's daily activities and mood. Dr Winona Tse, of Mount Sinai Movement Disorders Center in New York City, talked to Medscape about TD management.
TD prevention should be considered when prescribing dopamine receptor blockers. How can we prevent TD in clinical practice?
The first line of prevention would be to avoid using dopamine receptor blockers, but this is often easier said than done, as some antipsychotics might be the only effective treatment option for a patient. It is important to remember that dopamine receptor blockers include first- and second-generation neuroleptics and some antiemetic medications: metoclopramide and prochlorperazine.[1] For the treatment of nausea in patients undergoing chemotherapy, ondansetron is an alternative that doesn't block dopamine receptors. For patients who need antipsychotics, atypical antipsychotics with less dopamine receptor blockade, such as clozapine, are recommended options. It is also good practice to assess individual patient risk: older adults are at higher risk for TD[2] as are those with genetic susceptibility.[3,4,5]
What if there are no alternatives to dopamine receptor blockers?
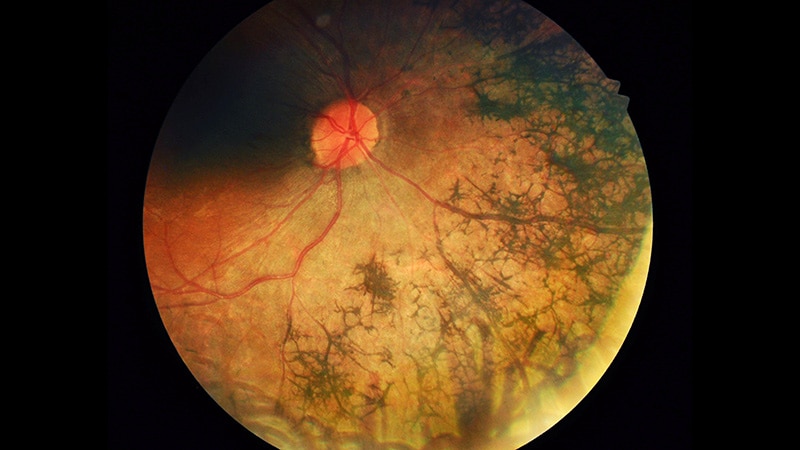
To minimize the risk for TD, it is recommended to use the lowest effective dose of that medication. In psychiatric settings, alternatives like SSRIs can be tried, but many patients, such as those with schizophrenia, need dopamine receptor blockers. Using less potent ones and minimizing dosage can help reduce TD risk.[6] Patients using dopamine receptor blockers should be monitored for TD periodically, with a thorough neurologic and physical exam. Most commonly, patients present with oral-facial movements like lip and mouth puckering, tongue protrusion, and jaw movements. TD can also affect the eyes with blinking and the limbs with uncontrollable movements. These movements can be choreiform or writhing.[1] While I don't routinely use scales in my practice, I have used the AIMS (Abnormal Involuntary Movement Scale) in clinical studies and for drug authorization purposes. Validated scales might be useful for long-term patient monitoring.
In case of a TD diagnosis, should the medication be suspended?
It's complicated. Based on the history of drug exposure, we can identify potential causes, but keep in mind that TD can occur after discontinuing antipsychotics, for example. Once a medication is identified, we can stop its use slowly or switch to a less potent one.[6] Collaboration with other specialists is key. I wouldn't stop a medication I didn't prescribe. Paradoxically, TD often improves with increasing the antipsychotic dose, but this isn't a long-term solution. If changing or reducing the dose isn't feasible, we should consider introducing another medication to control TD. Vesicular monoamine transporter 2 (VMAT2) inhibitors — deutetrabenazine and valbenazine — are the main drugs approved for TD treatment found to be effective in symptom reduction.[7,8,9] Possible side effects include sedation and parkinsonism, but they are generally well tolerated. Severe cases that don't respond to medication might be referred for deep brain stimulation (DBS); some studies showed significant improvement on the AIMS, but DBS is considered an off-label option.[7,8]
VMAT2 inhibitors are a great addition to the management of TD. What new developments do you expect to see in the next few years?
I am involved in the phase 4 IMPACT-TD study with Teva to assess the impact of TD and real-world use of deutetrabenazine (Austedo). This is a 3-year longitudinal multicenter study with two parts, including a registry that will collect information from TD patients about their condition, its impact and effect across domains including social, psychological, and physical function, and how TD progresses over time. The second part will evaluate deutetrabenazine in approximately 600 patients aged 18 or older from the registry. There has been significant enthusiasm among patients to participate, which also reflects the unmet need for more TD research.

.webp) 3 days ago
3
3 days ago
3
























 English (US)
English (US)